HFrEF WITH EF 33% SECONDARY TO CAD (LAD TERRITORY S/P? MI) WITH K/C/O DM 2 WITH TYPE 1 VITILIGO VULGARIS, ALLERGIC CONTACT DERMATITIS, AZTEOTOTIC ECZEMA
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 64 year male patient, teacher by occupation came to the OPD with chief complaints of
1. B/L lower limb edema since 1 month
2. SOB since 1 month
3. Hyper pigmented patches over both shins and both hands 10 days
HISTORY OF PRESENTING ILLNESS
The patient was apparently asymptomatic 1 month back. Then he developed b/l lower limb swelling. It was insidious in onset, gradually progressed from feet to thighs and also involving scrotum. There is also a H/o of reduced physical activity.
There is SOB gradually progressing from grade 1 to grade 3. Not associated with any orthopnoea, palpitations. Aggravated on walking and relieved on taking rest.
From 10 days, the patient is having hyper pigmented patches over front of the leg and on both hands. Not associated with itching, gradually progressive. No aggravating and relieving factors.
PAST HISTORY
1 month ago, he was diagnosed with COVID 19 and was admitted for 10 days and was then discharged. In Feburary, he had sudden onset cough and SOB early in the morning at 4:00am. He was admitted to hospital for 4 days and was adviced angiogram. But the patient was not willing and discharged.
K/C/O Type 2 DM (25 years), on OHA Glimy-M1 BD
Not a K/C/O HTN, CAD, TB, asthma.
PERSONAL HISTORY
Diet - Mixed
Appatite - Reduced
Sleep - Adequate
Bowel and bladder - Normal
Addictions - None
FAMILY HISTORY
None significant
GENERAL EXAMINATION
Pt is C/C/C
Moderately built and nourished
Afebrile
No pallor, icterus, cyanosis, lymphadenopathy, clubbing
B/L lower limb pitting edema. Hyper pigmented patches seen on both shins and hands.
BP 130/70 mmHg
PR 84 bpm
RR 22 cpm
SpO2 98% in room air
GRBS 126mg/dl
CVS
INSPECTION:
1. Shape of Chest Symmetrical, moving equally with respiration
2. Trachea position central
3. No visible pulsations seen
No scars, sinuses or dilated veins seen in any part of the thorax.
No bony abnormalities seen (Spine)
PALPITATION:
1- All inspector findings were confirmed.
2-Trachea is central.
3-Apex Beat confirmed to be in Lt 5th ICS 1cm lateral to MCL
PERCUSSION:
1. Rt border of heart corresponds to Rt sternal border
2. Lt border of heart corresponds to apex beat
3. Pulmonary areas on percussion
AUSCULATION:
S1 and S2 heard
RS
BAE +, clear
P/A
Soft
Non-tender
Bowel sounds heard
CNS
No focal abnormalities detected
Diagnosis
HFrEF WITH EF 33% SECONDARY TO CAD (LAD TERRITORY S/P? MI) WITH K/C/O DM 2 WITH TYPE 1 VITILIGO VULGARIS WITH ALLERGIC CONTACT DERMATITS WITH AZTEOTOPIC ECZEMA
Chest X ray
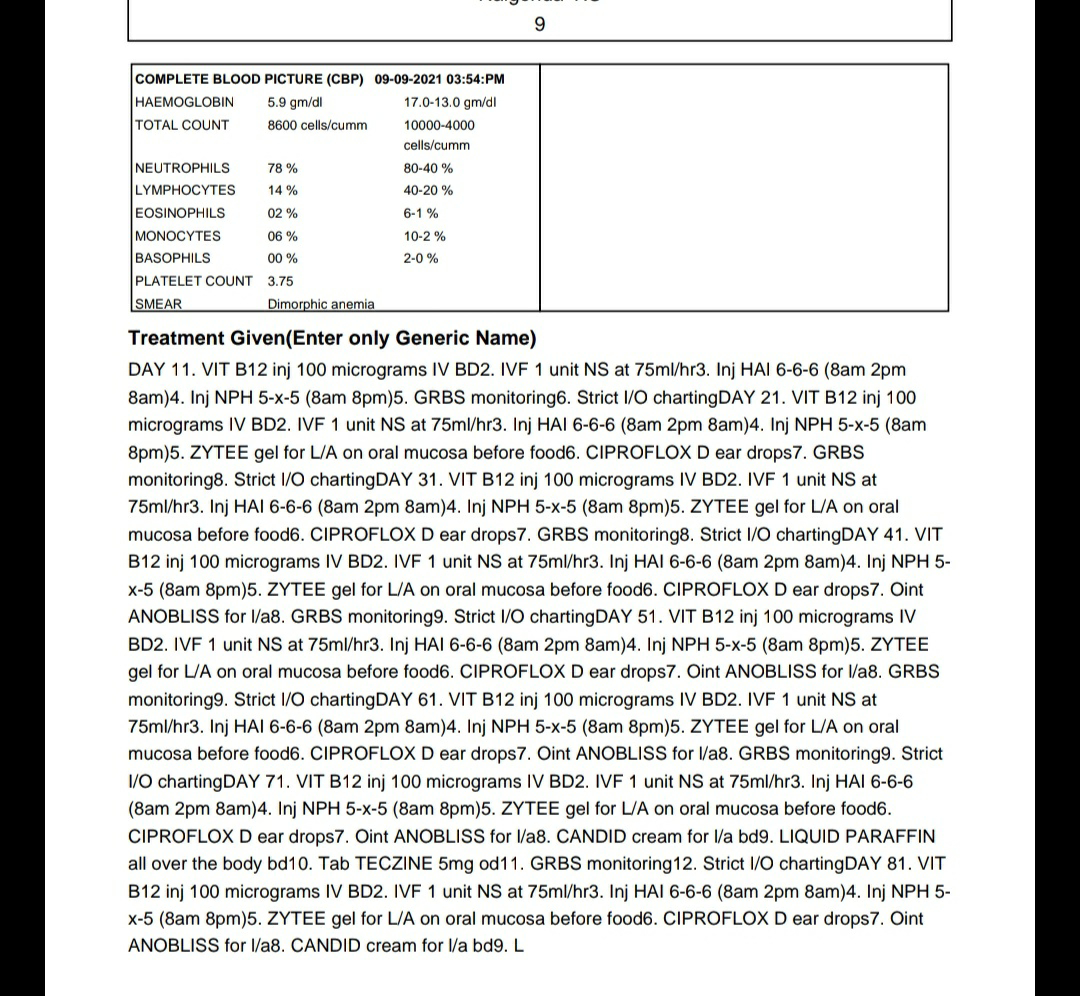
Hb
CUE
2D ECHO
HbA1c
LFT
RFT
ECG
DVL REFERRAL
DAY 0
SOAP Notes
Subjective
Patient c/o swelling and skin changes on limbs
Objective
Pallor -
Clubbing -
PR - 85 bpm
BP - 130/70mmhg
Afebrile
Spo2 - at 99% on RA
RR - 17 cpm
CVS - S1 S2 +
RS - BAE +
CNS - No FAD
Per Abdomen - Soft, non-tender, Bowel sounds +
HB 9.5
LFT
Albumin 2.8
Protein 4.6
A/G ratio 1.51
Total bil 0.88
Direct bil 0.19
SGOT 13
SGPT 10
RFT
Urea 5.9
Creatinine 1.8
Uric acid 1.4
FBS 79mg/dl
Assessment
HFrEF (EF 33%) secondary to CAD k/c/o type 2 diabetes with type 1 Vitiligo vulgaris with allergic contact dermatits with azteotopic eczema
Plan of treatment
1. Head end elevation
2. Tab DYTOR PLUS 10mg/po/bd
3. MOMATE cream for l/a od
4. MOISTUREX SOFT cream for l/a
5. Protein powder 2 tbsp in milk bd
6. Fluid restriction till 1.5 litres/day
7. Salt restriction till 2 g/day
8. OHA to be continued
9. BP charting
10. I/O charting
11. GRBS monitoring
Day 1
USG guided aspiration of ascitic fluid performed. 20 ml of fluid was removed. The removed fluid was sent for SAAG, ascitic fluid cell count, culture and sensitivity and gram staining.
SOAP Notes
Subjective
Patient c/o swelling and skin changes on limbs
Objective
Pallor -
Clubbing -
PR - 80 bpm
BP - 120/80mmhg
Afebrile
Spo2 - at 99% on RA
RR - 14 cpm
CVS - S1 S2 +
RS - BAE +
CNS - No FAD
Per Abdomen - Soft, non-tender, Bowel sounds +
GRBS MONITORING
22/08/21
8 AM 134mg
2 PM 111mg
8 PM 72 mg
23/08/21
8 AM 93 mg
Investigations
PLBS 94mg
Assessment
HFrEF (EF 33%) secondary to CAD k/c/o type 2 diabetes with type 1 Vitiligo vulgaris with allergic contact dermatits with azteotopic eczema
Plan of treatment
1. Head end elevation
2. Tab DYTOR PLUS 10mg/po/bd
3. MOMATE cream for l/a od
4. MOISTUREX SOFT cream for l/a
5. Protein powder 2 tbsp in milk bd
6. Fluid restriction till 1.5 litres/day
7. Salt restriction till 2 g/day
8. OHA to be continued
9. BP charting
10. I/O charting
11. GRBS monitoring
Day 2
SOAP Notes
Subjective
Patient c/o swelling and skin changes on limbs
Objective
Pallor -
Clubbing -
PR - 84 bpm
BP - 120/80mmhg
Afebrile
Spo2 - at 99% on RA
RR - 17 cpm
CVS - S1 S2 +
RS - BAE +
CNS - No FAD
Per Abdomen - Soft, non-tender, Bowel sounds +
GRBS MONITORING
23/08/21
8 AM 93mg/dl
2 PM 97mg/dl
8 PM 89mg/dl
24/08/21
8 AM 90 mg/dl
Investigations
Ascitic Fluid Analysis
Sugar 83mg/dl
Protein 2.2g/dl
Albumin 1.46g/dl
LDH 97 IU/l
SAAG 1.41
LFT
ALP 157 IU/L
Total Protein 5g/dl
Albumin 2.87g/dl
Assessment
HFrEF (EF 33%) secondary to CAD k/c/o type 2 diabetes with type 1 Vitiligo vulgaris with allergic contact dermatits with azteotopic eczema
Plan of treatment
1. Head end elevation
2. Tab DYTOR PLUS 10mg/po/bd
3. MOMATE cream for l/a od
4. MOISTUREX SOFT cream for l/a
5. GLIMIPERIDE 0.5 gm/po/od
6. Protein powder 2 tbsp in milk bd
7. Fluid restriction till 1.5 litres/day
8. Salt restriction till 2 g/day
9. OHA to be continued
10. BP charting
11. I/O charting
12. GRBS monitoring
Day 3
Tab Hydralazine was added to reduce the pedal edema.
SOAP Notes
Subjective
Patient c/o swelling (reduced) and skin changes on limbs
Objective
Pallor -
Clubbing -
PR - 89 bpm
BP - 120/80mmhg
Afebrile
Spo2 - at 99% on RA
RR - 14 cpm
CVS - S1 S2 +
RS - BAE +
CNS - No FAD
Per Abdomen - Soft, non-tender, Bowel sounds +
GRBS MONITORING
24/08/21
8 AM 90mg/dl
2 PM 131mg/dl
8 PM 89mg/dl
25/08/21
8 AM 122 mg/dl
Assessment
HFrEF (EF 33%) secondary to CAD k/c/o type 2 diabetes with type 1 Vitiligo vulgaris with allergic contact dermatits with azteotopic eczema
Plan of treatment
1. Head end elevation
2. Tab DYTOR PLUS 10mg/po/bd
3. MOMATE cream for l/a od
4. MOISTUREX SOFT cream for l/a
5. GLIMIPERIDE 0.5 gm/po/od
6. HYDRALAZINE 25mg/po/od
7. Protein powder 2 tbsp in milk bd
8. Fluid restriction till 1.5 litres/day
9. Salt restriction till 2 g/day
10. OHA to be continued
11. BP charting
12. I/O charting
13. GRBS monitoring
Day 4
SOAP Notes
Subjective
Patient c/o swelling (reduced) and skin changes on limbs
Objective
Pallor -
Clubbing -
PR - 87 bpm
BP - 120/80mmhg
Afebrile
Spo2 - at 99% on RA
RR - 16 cpm
CVS - S1 S2 +
RS - BAE +
CNS - No FAD
Per Abdomen - Soft, non-tender, Bowel sounds +
GRBS MONITORING
25/08/21
8 AM 122 mg/dl
2 PM 176 mg/dl
8 PM 163 mg/dl
26/08/21
8 AM 154 mg/dl
INVESTIGATIONS
24 hr urine volume 1700ml
24 hr urine protein 536.8 g
Assessment
HFrEF (EF 33%) secondary to CAD k/c/o type 2 diabetes with type 1 Vitiligo vulgaris with allergic contact dermatits with azteotopic eczema
Plan of treatment
1. Head end elevation
2. Tab DYTOR PLUS 10mg/po/bd
3. MOMATE cream for l/a od
4. MOISTUREX SOFT cream for l/a
5. GLIMIPERIDE 0.5 gm/po/od
6. HYDRALAZINE 25mg/po/od
7. Protein powder 2 tbsp in milk bd
8. Fluid restriction till 1.5 litres/day
9. Salt restriction till 2 g/day
10. OHA to be continued
11. BP charting
12. I/O charting
13. GRBS monitoring
Day 5
SOAP Notes
Subjective
Patient c/o swelling (reduced) and skin changes on limbs
Objective
Pallor -
Clubbing -
PR - 84 bpm
BP - 120/80mmhg
Afebrile
Spo2 - at 99% on RA
RR - 16 cpm
CVS - S1 S2 +
RS - BAE +
CNS - No FAD
Per Abdomen - Soft, non-tender, Bowel sounds +
Assessment
HFrEF (EF 33%) secondary to CAD k/c/o type 2 diabetes with type 1 Vitiligo vulgaris with allergic contact dermatits with azteotopic eczema
Plan of treatment
1. Head end elevation
2. Tab DYTOR PLUS 10mg/po/bd
3. MOMATE cream for l/a od
4. MOISTUREX SOFT cream for l/a
5. GLIMIPERIDE 0.5 gm/po/od
6. HYDRALAZINE 25mg/po/od
7. Protein powder 2 tbsp in milk bd
8. Fluid restriction till 1.5 litres/day
9. Salt restriction till 2 g/day
10. OHA to be continued
11. BP charting
12. I/O charting
13. GRBS monitoring
Day 6
SOAP Notes
Subjective
Patient c/o swelling (reduced) and skin changes on limbs
Objective
Pallor -
Clubbing -
PR - 81 bpm
BP - 120/80mmhg
Afebrile
Spo2 - at 99% on RA
RR - 18 cpm
CVS - S1 S2 +
RS - BAE +
CNS - No FAD
Per Abdomen - Soft, non-tender, Bowel sounds +
Assessment
HFrEF (EF 33%) secondary to CAD k/c/o type 2 diabetes with type 1 Vitiligo vulgaris with allergic contact dermatits with azteotopic eczema
Plan of treatment
1. Head end elevation
2. Tab DYTOR PLUS 10mg/po/bd
3. MOMATE cream for l/a od
4. MOISTUREX SOFT cream for l/a
5. GLIMIPERIDE 0.5 gm/po/od
6. HYDRALAZINE 25mg/po/od
7. Protein powder 2 tbsp in milk bd
8. Fluid restriction till 1.5 litres/day
9. Salt restriction till 2 g/day
10. OHA to be continued
11. BP charting
12. I/O charting
13. GRBS monitoring
Discharge Summary